ACT NOW: a new foot assessment tool for people with diabetes
7 July 2021 | Dr Anne Phillips, QN
We would like to encourage every Community Nurse to adopt and use the new ACT NOW foot assessment tool. Community Nurses, Nursing Home Staff and carers are at the forefront of helping people with diabetes and detecting foot problems. Any delay in treating a foot related problem in someone with diabetes can be catastrophic.
‘Time is Tissue’
iDEAL Diabetes is a Multidisciplinary team that aims to support and offer educational approaches and tools for every healthcare professional and every person with diabetes, to reduce variations in diabetes care. ACT NOW is designed as an easy-to-use assessment tool for practitioners working with people with diabetes who are affected by a foot problem. A key aim is to reduce delays in referral time for specialist review as ‘time is tissue’ in diabetes care.
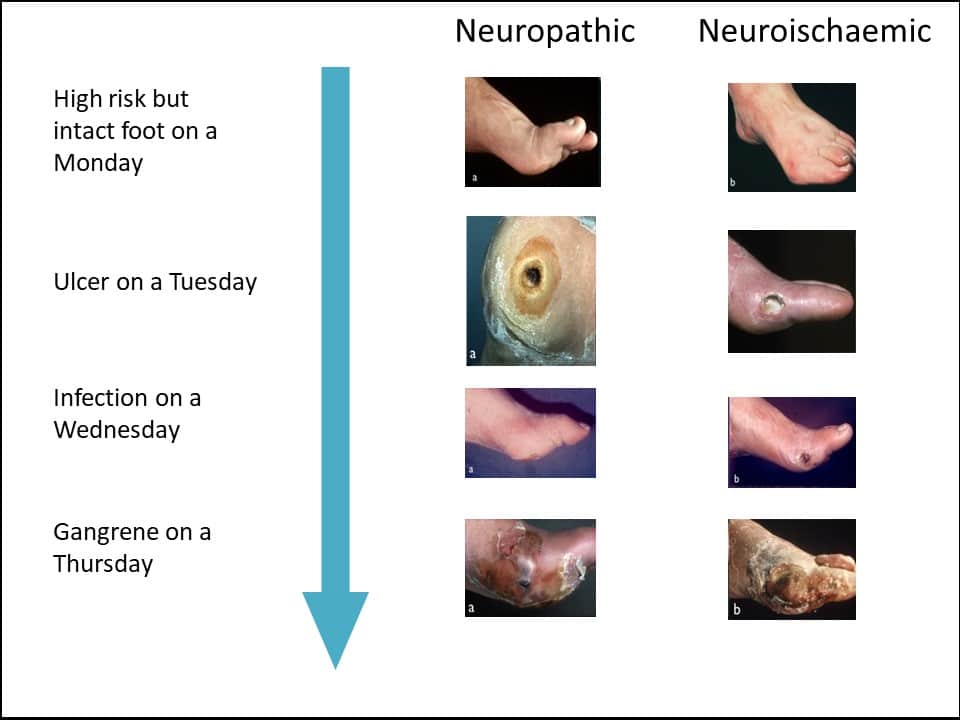
During their lifetime, one in three People with Diabetes may develop foot ulcers (Armstrong et al, 2017). These ulcers are highly susceptible to infection which can spread rapidly, causing overwhelming tissue destruction or gangrene, necessitating major amputation. The progression from an initial ‘scratch’ to gangrene can take as little as 48 hours. People can also lose a leg to gangrene because of a reduction in blood supply to the foot (National Diabetes Footcare Audit of England and Wales (NDFA), 2019).
A lack of knowledge can lead to a lack of urgency among People with Diabetes, carers and staff, who may not recognise that they have a foot related problem requiring urgent referral or care interventions (Pankhurst and Edmonds, 2018). A temperature change can indicate infection or the development of Charcot arthropathy. However, Charcot arthropathy can be easily missed without access to an X-ray or MRI scan, and thus may not receive a necessary urgent referral to a Multi-disciplinary Footcare Services Team (Vopat et al, 2018).
As well as amputation being a personal life-changing event, the financial burden of diabetes-related foot care is immense. The cost of health care for ulceration and amputation in diabetes in 2014–2015 was estimated at between £945 million and £1,087 million representing 0.8% to 0.9% of the National Health Service budget for England alone (Kerr et al, 2019). If there are difficulties in accessing a GP appointment for any reason, there is a risk of critical delay in People with Diabetes receiving appropriate assessment and treatment.
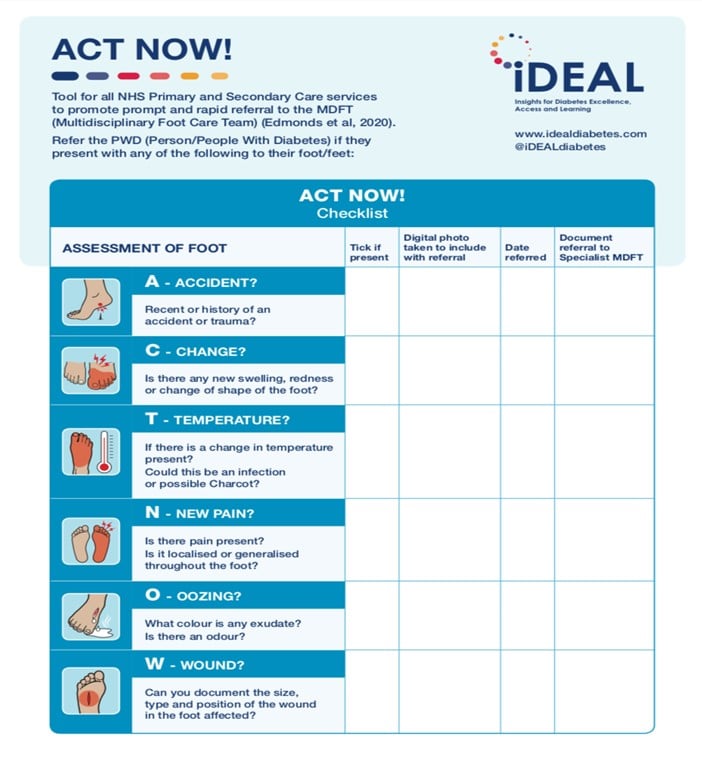
The iDEAL ACT NOW Assessment Tool
The iDEAL ACT NOW Assessment Tool is designed to promote timely referral and save limbs. iDEAL seeks to reduce amputations by 50% in 5 years by encouraging people to use the resource.
Assessing someone just before a weekend and being advised to delay until Monday or the following week for an assessment is not safe practice. Using ACT NOW, risks can be identified quickly, leading to more urgent referral to General Practice assessment, community podiatry or A&E if the local hospital does not have Multi-disciplinary Footcare Services in place. As illustrated in Figure 1 below (Edmonds & Foster, (2014)) a person’s foot can deteriorate within just five days to the point of needing amputation. Prompt assessment and early referral can help reduce this unnecessary suffering.
The ACT NOW Assessment Tool also seeks to reduce the stigma often experienced by People with Diabetes regarding complications and remove any blame or shame associated with diabetes complications. This includes not using the terms ‘Diabetic Foot or Diabetic Ulcer’ as these can add to the stigma experienced by People with Diabetes. These changes can be created through encouraging and enabling an environment of education, knowledge and trust using language that enables, not disadvantages People with Diabetes (Cooper et al, 2018).
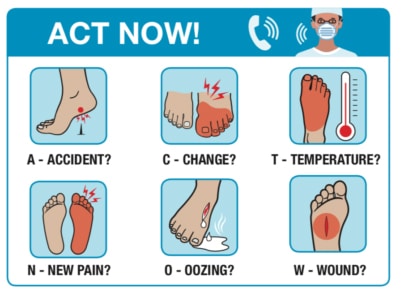
- A Recent or history of an accident or trauma?
- C Is there any new swelling, redness, change of shape of the foot?
- T If there is a change in temperature present? Infection or possible Charcot?
- N Is there new pain present? Is it localised or generalised throughout the foot?
- O What colour is any exudate (oozing)? Is there any odour?
- W document the size, shape and position of the wound in the foot affected?
The ACT NOW assessment tool is illustrated below:
National Policy
The NHS Long Term Plan (2020) commits to providing people with diabetes with access to specialist footcare services to improve recovery, reduce lengths of stay and future readmission rates.
NICE (NG19, 2019) has stipulated that within the community, everyone with diabetes should have an annual foot examination to detect their risk of foot ulceration. As part of this, they should be made aware of their risk and what to do if they develop a foot lesion. Anyone with an increased risk should be referred to a community footcare protection service (FPS). Anyone who is at high risk or has active ulceration should be referred to the Multidisciplinary Diabetes Footcare Service.
The GiRFT Report, (Rayman & Kar, 2020) identified deficits in Diabetes and foot care that affect people in many geographical areas. For example, some hospitals still do not have fully established MDFS to coordinate care of both inpatients and outpatients with footcare problems. GiRFT recognises the need to act on this as a matter of urgency.
ACT NOW has been endorsed by Diabetes UK, Juvenile Diabetes Research Foundation (JDRF), International Diabetes Federation (IDF), Diabetes Foot Care Networks UK, D-Foot International, The Royal College of Podiatry and was awarded the Diabetes UK Nursing and Allied Healthcare Professional Research Poster Award at Diabetes UK, (2021).
Please access the downloadable ACT NOW resources and guides on how to undertake a foot assessment with People with Diabetes via this link: https://idealdiabetes.com/act-now-education-resources/
Dr Anne Phillips, Queen’s Nurse, Co-Chair of iDEAL Diabetes, Associate Professor in Diabetes Care, Birmingham City University
References
Armstrong DG, Boulton AJM, Bus SA (2017) Diabetic Foot Ulcers and Their Recurrence. N Engl J Med 376(24): 2367–75
Cooper A, Kanumilli N, Hill J, et al. (2018) Language matters. Addressing the use of language in the care of people with diabetes: position statement of the English Advisory Group. Diabet Med. 35(12):1630–1634. doi:10.1111/dme.13705
Edmonds ME, Foster AVM (2014) Managing the Diabetic Foot. 3rd edition. Oxford: Blackwell Science
Kerr M, Barron E, Chadwick P, Evans T, Kong WM, Rayman G, Sutton-Smith M, Todd G, Young B, Jeffcoate W (2019) The cost of diabetic foot ulcers and amputations to the National Health Service in England .Diabet Med. Aug;36(8):995-1002. doi: 10.1111/dme.13973
NHS Digital (2019) National Diabetes Foot Care Audit, 2014– 2018. NHS Digital, Leeds. Available at: https://bit.ly/36i2T7J. (accessed 28.05.2021)
NHS England, (2019) NHS Long Term Plan, https://www.longtermplan.nhs.uk/
NICE NG19, (2019) Diabetic Foot Problems: Prevention and Management, https://www.nice.org.uk/guidance/ng19
Pankhurst C.J., Edmonds M.E., (2018) Barriers to foot care in patients with diabetes as identified by healthcare professionals Diabet Med, 35: 1072-1077
Rayman G, Kar P (2020) GiRFT Report Diabetes: Getting it right first time, https://www.gettingitrightfirsttime.co.uk/wp-content/uploads/2020/11/GIRFT-diabetes-report.pdf
Vopat ML, Nentwig MJ, Chong ACM, Agan JL Shields NN,Yang SY. (2018) Initial Diagnosis and Management for Acute Charcot Neuroarthropathy. Kans J Med. Nov; 11(4): 114–119

 Back to Blog
Back to Blog